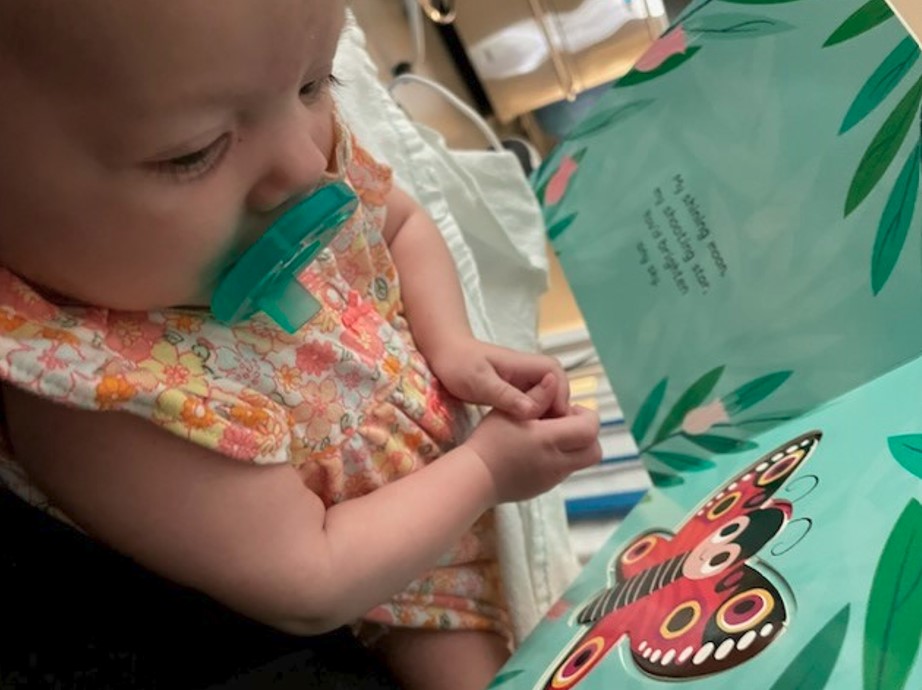
You wouldn’t know it to look at her today, but nine-month-old Penelope was given just a 25 per cent chance of surviving her congenital diaphragmatic hernia (CDH).
She was still in her mother’s womb when the doctors discovered the potentially fatal abnormality.
“When I went for my 19 week gender scan, that’s when they saw Penelope’s stomach in her chest. That was the first indication that there was something wrong,” says mother Chelsea Belleau, who works as a kindergarten teacher in Surrey.
“Obviously we were devastated. We were referred to maternal fetal medicine at BC Women’s and they confirmed she had CDH.”
CDH occurs when there is a hole in the diaphragm so that other organs, including the bowel, stomach, and even the liver can move into the chest cavity, which limits space for the lungs to grow properly, and can result in respiratory complications.
BC Children's Hospital and BC Women's Hospital + Health Centre (C&W) are the only hospitals in the province that treat the condition.
“We were basically told that many babies don’t survive and that she may need an operation performed in Toronto,” says Belleau. “But first, they had to figure out the severity. They discovered her right lung, which was supposed to be her good lung, was very tiny so they put her in the ‘severe’ category.”
 C&W Chief of Surgery Dr. Erik Skarsgard oversaw Penelope’s case and says what C&W does well is not only diagnosing the actual condition, but also estimating the severity of difficulties after birth.
C&W Chief of Surgery Dr. Erik Skarsgard oversaw Penelope’s case and says what C&W does well is not only diagnosing the actual condition, but also estimating the severity of difficulties after birth.
“Our maternal fetal medicine specialists at BC Women’s used a combination of ultrasound and fetal magnetic resonance imaging to estimate the severity of lung underdevelopment,” he says.
“The likelihood of her dying after birth from severe lung underdevelopment was pretty high.”
The family travelled to Toronto, where they remained for six weeks. When Chelsea was at 29 weeks gestation, doctors placed a small camera into her womb and a balloon in Penelope’s windpipe. That balloon created forces in the trachea that caused both lungs to grow rapidly, increasing chances of survival after birth. At 34 weeks, they took the balloon out.
“There was a big risk of going into preterm labour, which would be fatal for Penelope,” says Belleau. “I was scared, but I knew this was going to save her life.”

Chelsea returned home to Richmond, B.C. and she was supposed to be induced to give birth at 38 weeks, but she went into labour a few days before that date. After 24 hours of labour, Penelope was born.
“Apparently it’s better to have a natural birth because when she is being pushed out, it pushes out the fluid around her lungs,” she says. “I got to hold her briefly and then they whisked her away with my husband. I think there were about 20 to 25 people in the birthing room. They had her intubated and they were manually keeping her alive until she went to the neonatal intensive care unit (NICU).”
Penelope was very ill and on a specialized respirator. At four days old, doctors decided to do the repair surgery on her diaphragm.
 Dr. Shahrzad Joharifard performed the surgery on Penelope. It was supposed to take five hours, but the family received a call just after three hours.
Dr. Shahrzad Joharifard performed the surgery on Penelope. It was supposed to take five hours, but the family received a call just after three hours.
“We thought, oh my goodness, something went wrong. They’re calling us too quickly, but basically, it went well. She was missing most of her diaphragm. They put a Goretex patch to replace her diaphragm and they put her organs back.”
“She sailed through everything pretty unscathed,” says Skarsgard. “She’s really a miracle story when you consider how slim her chances of survival were when she was first diagnosed.”
 Penelope returned to the NICU to recover, spending a total of 126 days there.
Penelope returned to the NICU to recover, spending a total of 126 days there.
“It’s a big, integrated team that’s involved in the care of CDH at C&W,” says Skarsgard. “We see about eight babies with CDH each year and the birth of each baby mobilizes our CDH team with pediatric surgery, neonatology, anesthesia, cardiology, pediatric ICU, specialty nursing and respiratory therapy all involved.
"We use locally developed treatment guidelines to encourage standardization of CDH care. The CDH team meets twice a day in the NICU during the critical phases of treatment, both before and after surgery. Because we were aware of how serious Penelope’s case was before she was born, we were prepared and she quickly became a focus for us.”
 The team at C&W co-developed an app, called the Canadian CDH Collaborative, for providers to follow the recommendations in the guidelines with a checklist. This standardization of care has been shown to improve outcomes for complex conditions like CDH, and has proven to be so popular, these guidelines are now widely used in other children’s hospitals across Canada and internationally.
The team at C&W co-developed an app, called the Canadian CDH Collaborative, for providers to follow the recommendations in the guidelines with a checklist. This standardization of care has been shown to improve outcomes for complex conditions like CDH, and has proven to be so popular, these guidelines are now widely used in other children’s hospitals across Canada and internationally.
Penelope now uses other muscles to breathe, as opposed to her diaphragm. The hope is that as she grows, the muscles around the Goretex patch in her diaphragm will continue to grow. She’s on a BiPAP (Bi-Level Positive Airway Pressure) machine at night and she has a feeding tube, but Chelsea says she’s doing well and praises the staff and physicians at C&W.
“They are amazing. They saved our daughter's life.”
